I love that LSVT BIG Program® is determined to help OT practitioners learn evidence based treatment strategies to help clients that have Parkinson’s Disease (PD). In this article we will dig into the what and how occupational therapy practitioners can use this program with our patients.
What does LSVT BIG Stand For?
LSVT BIG program stands for “Lee Silverman Voice Treatment” BIG, and it is a specialized program designed to enhance motor skills and movement for individuals diagnosed with Parkinson’s disease.
What is LSVT BIG Treatment?
Per their website, “LSVT BIG is a standardized treatment protocol, which is customized to the unique goals of each patient including both gross and fine motor skills. LSVT BIG can be adapted or progressed in order to meet each patient’s needs across a range of disease severity and presenting impairments.”
LSVT BIG protocol treatment consists of:
1) 16 sessions: 4 consecutive days a week for 4 weeks
2) Individual 1 hour sessions
3) Daily homework practice
4) Daily carryover exercises
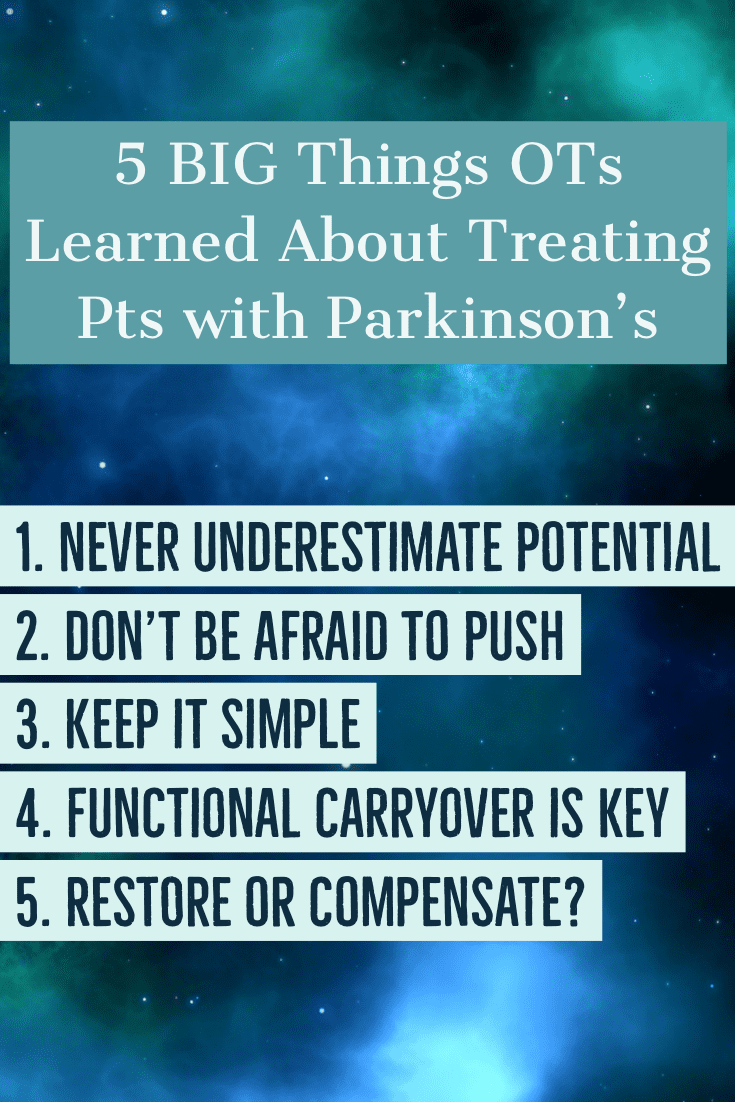
Let’s dig into 5 ways that the LSVT BIG Program helps occupational therapy practitioners get results with our patients.
1. Never Underestimate Your Patient’s Potential
When you evaluate a person who has had PD for a long time, one of the first things you might notice is a flat affect, followed by a bit (or a lot) of difficulty in getting up from a chair, a slow, shuffling gait and flexed posture. It would be easy to make a quick judgment about that patient’s potential (or their desire to even be in therapy!), but time and time again, we are surprised at what can be magically unlocked with therapy.
“I remember a gentleman who arrived for his first OT appointment with a less than enthusiastic facial expression” says Erica. “He was walking very slowly with a quad cane and had a propulsive, shuffling gait pattern. After evaluating him, it was apparent to me that he was able to move bigger and better when cued, so I knew he’d be a good candidate for LSVT BIG.”
Over the course of the of intensive LSVT BIG treatment, four times a week for four weeks, his attention to amplitude greatly improved his safety with functional mobility to the point where was able to walk again with complete confidence and without a cane. I was shocked not only by his potential to improve his mobility, but also by the profound effects it had on his mood and facial expression. I realized that I had initially misjudged his ability and motivation based upon his facial masking, but was glad I decided to give him the benefit of the doubt!”
Video – Gait in a man with PD before and after LSVT BIG program training
2. Don’t Be Afraid to Push Your Patient
This really goes along with the first point. Your patients with PD have great potential, but the only way to fully realize that potential is by not being afraid to “push them” during LSVT therapy exercises. You are likely familiar with key principles which can help to drive neuroplasticity and motor learning from your neuro coursework or from reading current literature. Exercising intensively is one key principle which has been found to be very important in people with PD. Even though we might know these principles in our heads, applying them in real world practice is often a challenge!
Before taking the LSVT BIG Training and Certification Course, the three of us agreed that it would have taken us out of our comfort zones to really push a patient who appears to be somewhat frail due to the symptoms of moderate to advanced PD. Now we understand not only the untapped potential they have, but how necessary it is to provide treatment that is sufficiently intensive and includes a high amount of practice to make lasting gains.
And – just like the research shows – it really does work!

On the other end of the spectrum are those patients who are so high functioning, that prior to a LSVT BIG program, we may have simply provided instruction in a home exercise program and discharged them.
Why?
Unless you know how to “unmask” the deficits, it is not always easy to see how those subtle symptoms can impact our patients’ occupational performance both now and in the future. Furthermore, we did not appreciate the severity of the underlying neuropathology that begs us to use intensive exercise to potentially slow symptom progression and delay disability.
A long-time patient who owns a successful landscaping business initially doubted the effectiveness of LSVT BIG treatment due to experiencing minimal difficulties. However, he was motivated to continue working full time despite Parkinson’s disease progression. Upon examination, it was discovered that he had mild hypokinesia, bradykinesia, and rigidity on his left side, putting him at risk of using his left hand less. With the goal of maintaining his job responsibilities, he embarked on the treatment.
In therapy, he practiced many functional work-related activities which require dual tasking and an extra layer of resistance and high-level balance challenges was added as it was relevant to his work demands. With this complex, purposeful and intensive training his confidence improved greatly. He felt empowered to continue to face the challenges of his job and to live well with PD. Since then, he has come back several times for a ‘tune-up’, and each time he has been able to tolerate even more challenges which were added to his home program.
3. Keep it Simple
One thing many people do not fully understand is just how skewed perception of movement and posture is in people with PD! Internally, people with PD often feel like they are moving quite normally, when indeed, it is obvious to us that they are moving too small or too slow. Additionally, cognitive and executive functioning changes common in PD often impact the ability to attend to more than one cue or attend to complex cues. As we reflect on the wordy and complex explanations we used to provide when training our patients how to get up from a chair or don their jacket, for example, we now say “No wonder carryover was so challenging!”
We have since learned to keep our verbal cues very simple and redundant when providing LSVT BIG, focusing on a singular target of amplitude during exercise and functional training. The goal in LSVT BIG is to re-calibrate a person’s perception of movement so they can use this simple internal cue of “BIG” in everyday life no matter what the task.
When we really began to implement this approach, the results were remarkable. In many patients self-cueing mechanisms could actually be restored! They began to detect and correct their errors before we could open our mouths. We unanimously agree that this new way of teaching spilled over into other treatments we provided, making us more effective OTs than ever before.
4. Functional Carryover is Key!
Do you hypothetically talk about functional carryover or do rote exercises with the hope that improved function will naturally result?
Not surprisingly, the best way to improve occupational performance is to practice the actual task.
To do this, we really need to dig in to discover:
- What activities and occupations are the most meaningful and most important to the patient – and the patient alone (i.e. not the spouse, friend, relative, neighbor, etc.).
- What brings them joy?
- Take the time to identify and train these activities has made all the difference in our treatment outcomes, our patients’ motivation and engagement not only during therapy, but with their home exercise programs as well.
In LSVT BIG, we assign something called daily Carryover Assignments as a way to mandate the use of bigger, better quality movements in everyday life outside of therapy. For example, a person one of us worked with recently had planned to babysit her grandchildren and take them to the park one afternoon. She and the patient decided to assign “BIG pushing” of the swing with both hands to address the hypokinesia, while challenging her balance at the same time. This was enjoyable and meaningful to the patient and began to help her generalize what she learned in therapy to her life outside of therapy.
5. To Restore or Compensate? That is the question…
You probably hear the phrase “Exercise is medicine” frequently if you are an OT who works with older adults. Since we know this to be true from countless studies on the physiological benefits of exercise, we also know that exercise and early referral to therapy can help to slow down symptom progression in PD, restore function, and in some cases, temporarily eliminate disability. This is exciting considering that in the not too distant past, improvement in neural function in PD was thought to be impossible; bypassing the deficient basal ganglia had been our only hope. No more!
From another angle on this word “compensatory,” OTs have always been geniuses in teaching patients how to use adaptive devices and clever compensatory techniques. While this is still true, one thing we all learned is that the use of adaptive devices may not even be needed in many cases!
For example, if we can adequately address the underlying deficit of hypokinesia by driving amplitude needed for a task such as buttoning, the patient can then perform this task without having to learn how to use buttonhook or avoid buttons altogether. And isn’t this what most patients ultimately desire – to simply do things the way they’ve always done them?
Video – Improving ability to button in less than 2 minutes
How has the LSVT Big program impacted your practice when working with patients that have Parkinson’s Disease?
About our guest bloggers:
Erica Vitek MOT, OTR, BCB-PMD, PRPC received her Master’s in Occupational Therapy from Concordia 

Bernadette Kosir OTR/L, CAPS is a graduate of University of Michigan in Ann Arbor and Wayne State 

Julia Wood, MOT, OTR/L received her Bachelor of Science in Exercise Science and Wellness from Ball 






7 thoughts on “5 Ways the LSVT BIG Program Helps Patients With Parkinson’s”
I was once certified in LSVT Big! I LOVED the program! The training was fantastic. My job changed and I didn’t have a need to continue my certification, but I have referred several clients to the website to find a therapist.
Thanks Kristina! I have not done the certification, but everyone I know that has it, LOVES it!
Pingback: 5 “BIG” Things We Learned About Treating Patients with Parkinson’s | Seniors Flourish
Hello Miss Mandy Chamberlain,
I’ve been meaning to post a shout-out to you and your many brilliant guests for a while now. My name is Cassie Greco. I am a first-year student in the OTD program at the College of Saint Mary in Omaha, NE. This is the school’s first OTD class and I could rave on and on about the faculty, my peers, and their unique program design. It’s something I’m passionate about!
In the past year, I have begun listening to the Senior Flourish Podcast and just devour the conversations. I enjoyed this particular podcast for a number of reasons. The first reason being my first encounter with LSVT BIG. A physical therapy mentor of mine was the first to tell me about LSVT BIG. She allowed me to observe a session with her and a very wonderful patient – motivated, musical, and devoted to his wife for many years. I couldn’t have had a better first encounter!
Much later I learned about RockSteady Boxing and had the opportunity to participate in a session with a physical therapist and occupational therapist here in NE. They are doing a phenomenal job leading the class and have created an awesome community!
The second reason that I love this podcast is Miss Bernadette Kosier’s comparison of OT to MacGyver. I have also felt that OT is such a large assortment of intellect and skills. The ingenuity that goes into problem-solving and tailoring therapy to fit each individual is part of what attracted me to the profession. I myself, love to dabble in many things and want to do so in many more things. Over and over again I can’t help but think that there just aren’t enough hours in a day for me to do everything that I want to do and learn everything that I want to learn.
The third reason I love this podcast is probably Miss Wood’s (?) follow-up comment and shout-out to her clinical educator Donna K. Heinle: “A good occupational therapist should be able to show up with a stick of gum, a ballpoint pen, and paper clip, and be able to lead an entire therapy session.” I will also never forget this. It’s too funny and such a great analogy to describe the profession.
Thank you again for the good quality topics you bring to your listeners and thank you especially for the educational component! Please continue the work that you do!
Cassie – This made my day! thank you so much for listening to the podcast. My goal is to share the #OTlove and knowledge so we can all be better clinicians. 🙂
Just completed my certification and LOVE the program! Trying to get started offering mobile outpatient (Med B) for Parkinson’s patients in my area.
What a great business plan Katherine!